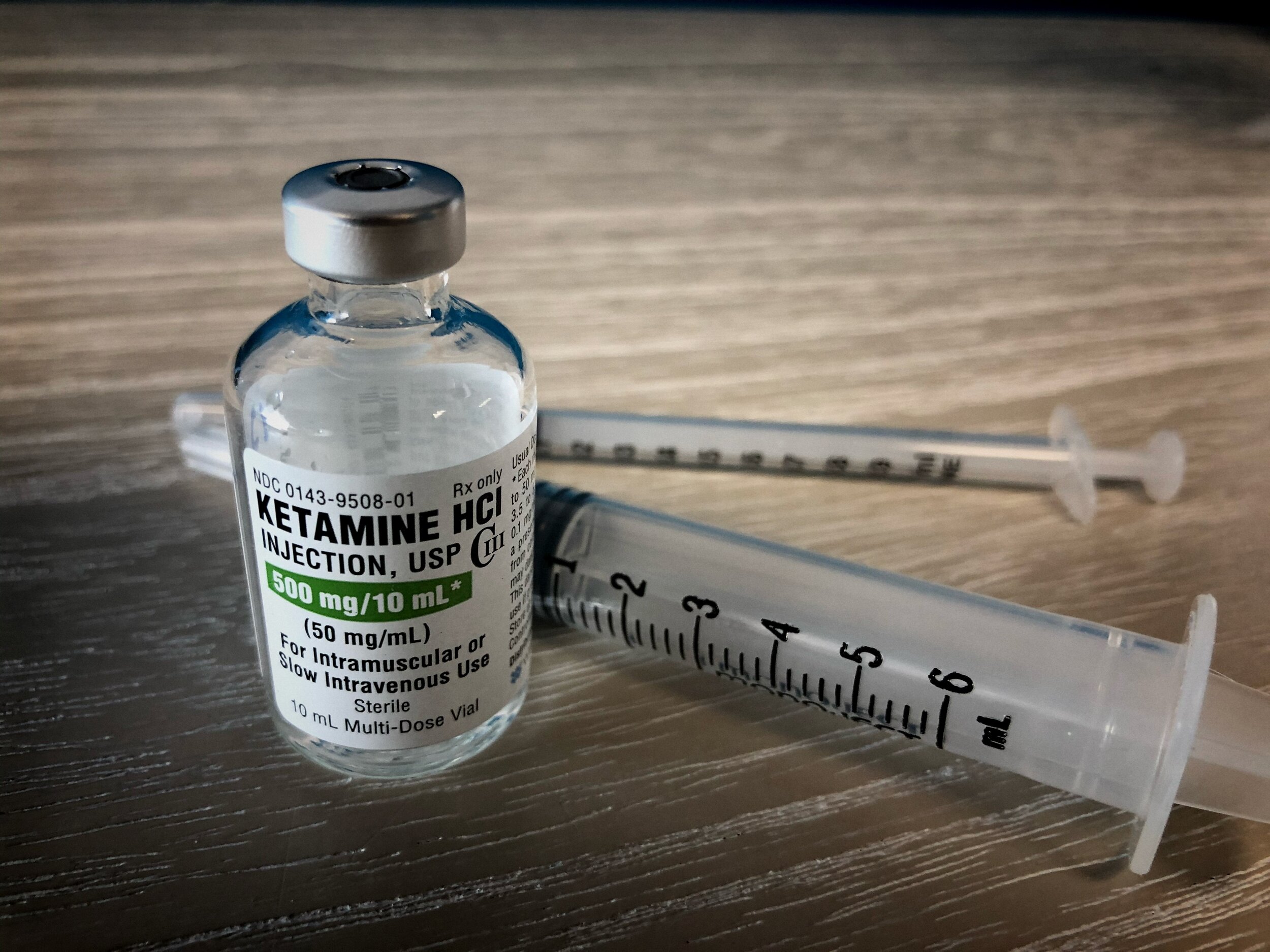
Music for Ketamine Therapy
A comprehensive guide for clinics
Are your patients watching TV or YouTube during their infusion sessions?
Do you question whether the music your patients listen to influences their therapeutic outcomes?
Do they bring their own music along?
Are you hesitant or unsure about offering guidance on music choices?
Are you searching for ways to enhance your approach to music in your practice?
If you nodded along to any of these questions, this article is written for you. We will investigate the existing approaches, answer the questions we are frequently asked, and aim to empower your decision making around music for your ketamine clinic.
To answer this question, we firstly need to consider the two distinct approaches that have evolved for treating persistent mental health conditions with ketamine – and how they are different.
Ketamine Therapy (KIT): This approach follows the traditional biomedical model and is typically offered at ketamine infusion clinics. This pharmacological approach is usually referred to as Ketamine Therapy or Ketamine Infusion Therapy (KIT), and is often overseen by certified providers in anaesthesiology or pain management. Patients are closely monitored throughout the process, including vital signs like blood pressure and heart rhythm, and typically leave the clinic approximately one hour after the ketamine administration. In this setting, psychotherapy is not typically part of the treatment plan.
Ketamine-Assisted Psychotherapy (KAP): This approach takes a more interdisciplinary and psychotherapeutic approach. Therapists, psychologists, and psychiatric providers collaborate closely with patients before, during and after the psychoactive phase of ketamine administration. KAP focuses on helping patients to process emotions and insights that emerge during their ketamine experiences, and learn how to apply them to their daily lives.
One might surmise that the primary distinction between these two approaches lies in the inclusion of psychotherapy. While this perspective holds true on the surface, a more crucial disparity becomes apparent when we delve into the fundamental assumptions that underlie each approach’s therapeutic mechanisms.
While Ketamine Infusion Therapy (KIT) emphasises that therapy improvements primarily result from neuropharmacological effects, and resulting changes in biochemistry; Ketamine-Assisted Psychotherapy (KAP) posits that these improvements are primarily mediated via shifts in subjective experience.
This article is not intended to undermine or oppose either approach; instead, its purpose is to begin by highlighting that taking a divisive stance, polarising KIT against KAP, could severely restrict both approaches from integrating the latest scientific insights into what constitutes effective mental health care.
Increasing bodies of research are suggesting that ketamine’s therapeutic potential lies in its combined neuropharmacological and subjective effects. If your clinic hasn’t yet harnessed the power of integrating insights from both perspectives, you could be significantly limiting the comprehensive benefits ketamine therapy can provide to your clients. If you are on the fence about this statement, please keep reading.
Numerous clinical studies have illuminated the antidepressant potential of a single sub-anesthetic dose of ketamine, particularly in treatment-resistant patients. Recent preclinical research endeavors have concentrated on unraveling the intricate molecular mechanisms that underlie ketamine’s distinctive antidepressant properties.
There are various hypotheses regarding the mechanism of ketamine’s antidepressant action. These hypotheses include direct inhibition of NMDA receptors (NMDARs) and the involvement of activating AMPA receptors (AMPAR).
Furthermore there are intricate connections demonstrated between ketamine’s antidepressant effects and downstream mechanisms governing synaptic plasticity. Ketamine directly stimulates the release of neurotrophins, a family of proteins that play a crucial role in the development, maintenance, and survival of neurons. These proteins are essential for the growth, differentiation and survival of neurons during both early development and throughout an individual’s life.
It’s important to recognise that these proposed mechanisms do not exist in isolation; rather, they likely collaborate to induce acute alterations in synaptic plasticity, ultimately resulting in the sustained strengthening of excitatory synapses—an essential prerequisite for the manifestation of antidepressant behavioural effects.
Increasing numbers of clinical studies directly highlight a compelling connection between specific subjective experiences induced by ketamine and an enhanced therapeutic response. These experiences, encompass ego dissolution, peak experiences, autobiographical insight, and mystical-like experiences – collectively referred to from here on as ‘experiences of personal significance’ (EPS).
Several hypotheses have been put forth to elucidate the intricate relationship between EPS and the amelioration of mental well-being. One prominent theory posits that ketamine (like classic psychedelics) can induce a ‘hyper-plastic’ state, facilitating rapid and profound learning that may lead to enduring psychological transformation.
Furthermore, related hypotheses delve into the significance of implicit learning in behavioural change. Implicit learning, defined as ‘learning by experiencing,’ was first elucidated by Nobel laureate Eric Kandel. It suggests that certain behaviours or information processing patterns can only be effectively learned and altered through direct experience (for example: one only learns how to walk, by walking).
This concept not only helps explain the efficacy of exposure-based therapies for conditions like PTSD but also provides a framework for understanding the mechanisms behind psychedelic therapies, including Ketamine-Assisted Psychotherapies.
The sustained therapeutic effects of ketamine are increasingly attributed to the emergence of a hyper-plastic brain and mind state, resulting in an accelerated rate of implicit learning and potentially paving the way for fundamental and lasting changes in mental health.
Therefore, in this context the primary question for care-providers working with ketamine is what are the implicit learning experiences offered to patients while they experience this “hyper-plastic” state?
This guide serves a dual purpose. Firstly, it seeks to highlight that the division between KIT and KAP approaches is not only unproductive but also lacks a scientific foundation. Secondly, it endeavours to provide a range of ideas and recommendations for seamlessly integrating these insights into your clinical practice when working with ketamine.
Multiple neuroimaging studies have demonstrated that the primary dissociative and ego-dissolution effects of ketamine correlate with the transitory disintegration and desegregation of hierarchical high-level brain network nodes (within the salience networks (SN)). This is hypothesised to account for the ‘dissociative’ state induced by ketamine, while a similar process within the default-mode network (DMN) explains its ‘psychedelic’ effects.
In the realm of KAP and psychedelic-assisted psychotherapy, the relaxation of deeply ingrained beliefs, with the support of psychotherapeutic guidance, is thought to pay pave the way for a revision of pathological self-representation models, with neuropharmacological stimulation of neuroplasticity playing a permissive role in this process of change.
The integrative framework presented here offers a rationale for harnessing the psychedelic properties of ketamine to enhance its enduring therapeutic benefits. It acknowledges that while ketamine’s immediate impact on the brain contributes to acute mood improvement, its lasting advantages are rooted in its temporary influence on neuroplasticity, the re-configuration of brain networks and the implicit learning that is paired with this.
It is imperative to underscore that the potential for enhanced implicit learning, within the hyper-plastic state induced by acute ketamine experiences, hinges on patient engagement. What individuals choose to engage with during this state will decisively mould the strengthening or weakening of neural pathways and information processing within the brain.
This aligns with one of the most fundamental and widely recognised principles of neuroplasticity and learning: neural pathways are reinforced solely through activity-based engagement.
In summary: while a patient may indeed experience an improved mood for hours or even days following ketamine administration while engaged in passive activities like watching the latest Netflix episode, such improvements may not fully represent the potential for lasting changes through implicit learning mechanisms. Care providers bear the responsibility of consciously creating an environment that fosters positive implicit learning experiences during Ketamine therapy.
Music offers an accessible, scalable, cost-effective, and highly efficient solution to introduce experience design into your clinic, all without the need to overhaul your operational structures or hire new staff.
Music wields remarkable influence over our subjective experiences. Dr. Mendel Kaelen, PhD., the founder of Wavepaths and distinguished neuroscientist, has conducted extensive research on the neurological and therapeutic underpinnings of music in the realm of psychedelic-assisted psychotherapy.
In essence, this research strongly indicates that carefully selected music has the potential to enhance the likelihood of triggering ‘experiences of personal significance’ (EPS), which, in turn, lead to more sustained therapeutic benefits. Conversely, when the music is ill-suited (we’ll define the criteria for ‘right’ and ‘wrong’ music elsewhere), there may be no improvement, or the clinical condition could even deteriorate.
Through ongoing research initiatives at Wavepaths, we’ve amassed evidence from thousands of sessions demonstrating that specific musical experiences significantly correlate with remission. Dr. Kyle T. Greenway, a psychiatrist and assistant professor at McGill University, and his team are pioneering the first clinical trials exploring the role of music in ketamine therapy. Emerging findings have shown that music can render ketamine therapy more tolerable psychologically and physiologically – e.g., by blunting ketamine’s well-known blood pressure increasing effects. Ongoing analyses are exploring how music experiences with ketamine can have important therapeutic impacts.
There is no universally perfect playlist for all clients. What might be a transformative experience for one could be distressing for another. Furthermore, the natural fluctuations in a person’s state from day to day mean that a music selection that enhances one session may prove disastrous in another.
When choosing music for patients undergoing ketamine therapy, it’s essential to take several variables into account. Research has identified three key factors in patients’ subjective experiences with music that are closely associated with sustained remission:
- Liking: Patients should genuinely enjoy the music chosen for them.
- Resonance: The music should resonate with the patient’s emotional state, creating a meaningful connection.
- Openness: Patients should feel open to the experiences evoked by the music, allowing them to engage fully.
This analysis carries significant implications for the use of music in ketamine therapy. Tailoring the music to individual preferences, rather than adopting a ‘one-size-fits-all’ approach, is paramount.
While playlists have been a part of psychedelic therapy for decades, there are legal, ethical, and therapeutic considerations to be aware of.
Using consumer music streaming services like Spotify in professional therapeutic settings violates terms of use and overlooks the contribution of artists to the therapeutic experience. Playing music that is too familiar or is not optimised to support altered states of consciousness can also reduce the therapeutic potential of the session.
While we wholeheartedly support the adoption of a person-centred approach, it’s important to acknowledge the potential challenges that can arise when patients are given complete autonomy over their music selection:
- Familiarity: Music that is widely recognized often brings strong predictability and carries well-established associations. This familiarity can impede the surrender of control and the facilitation of new implicit learning experiences.
- Mismatch: Music that is enjoyable in a sober state of consciousness may prove perplexing and unsupportive in the context of the ketamine experience.
This is why Wavepaths was founded: to simplify music selection for therapeutic work. All Wavepaths’ music is created based on its ongoing research program, specifically optimised for ketamine therapies, and designed to be easy to implement and used on a daily basis.
While we understand that the lowest cost doesn’t always equate to the best value, we acknowledge the economic considerations in clinic management.
Without a doubt, we have become both the most budget-friendly and legal music platform for clinical purposes. If you come across more cost-effective and fully licensed options, we encourage you to bring them to our attention.
We firmly believe that when clinics invest in enhancing the patient experience, it leads to tangible benefits for both patients and the clinic. We therefore extend an invitation for you to explore Wavepaths at no cost, allowing you to personally assess its impact on your patients. Plus, we offer a no-questions-asked money-back guarantee, ensuring your satisfaction with our service without any financial risk.